Venous Ulcers
Conveniently located to serve the areas of Westlake, OH

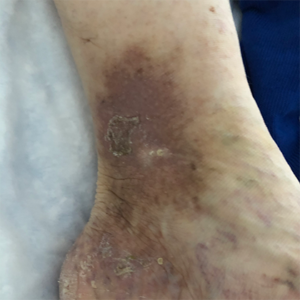
Venous Ulcers are painful, unsightly open sores in the lower legs that are primarily caused by chronic venous insufficiency (CVI), or poor circulation and blood flow in the legs. Veins are the blood vessels responsible for moving deoxygenated blood back to the heart. In patients with CVI, blood cannot be adequately directed back toward the heart because the valves in the veins are damaged.
Venous Leg Ulcers (often abbreviated to VLUs) are defined as open lesions between the knee and ankle joint that occur in the presence of venous disease and affect approximately 1% of the US population.(1)(2) Their speedy treatment is of utmost importance for patient safety and comfort. A skilled vascular surgeon can choose from a selection of treatment options for VLUs, depending on the patient’s individual needs and medical history. These fall into four main categories:
- Conservative Management
- Treatment with Medication
- Debridement
- Surgical Intervention.
Don’t delay getting the venous ulcer treatment you need a moment longer! With over 35 years of experience treating venous ulcers, varicose veins, spider veins, and leg swelling among other conditions, you can trust Dr. David Naar to alleviate the situation with professional medical care of the highest quality. To book your consultation with an experienced professional in the field of vascular health Dr. Naar, please get in contact with Premier Vein Clinic at (440) 641-0433 at your earliest convenience.
Contents
Before and After Photos
Venous Ulcer Symptoms in the Legs
The circulatory system plays a vital role sending oxygen, blood, and nutrients, to where they need to be in the body. When flow is reduced, blood can pool, and pressure increases in the veins, causing damage. This continuing pressure can make your skin more fragile and increase the likelihood of breakage after a simple knock or scratch. Unfortunately, these physical processes can culminate to create the “perfect storm” of negative factors, resulting in venous ulcers in the ankle and lower leg. Knowing the signs and symptoms of VLUs is the first step toward getting swift treatment.
Early Signs of Venous Ulcers:
Symptoms of Venous Ulcers:
- Shallow sore with a red base, yellowness
- Unevenly shaped borders
- Shiny/tight/warm/hot/discolored skin
- Pain in the entire leg
- Bad odor and pus (more serious infection)
VLUs & Stasis Dermatitis
Sores that won’t heal and swelling around your ankles are sometimes symptoms of venous ulcers, or another similarly presenting condition called stasis dermatitis. The two conditions occur when you have poor circulation in your legs and feet. Although they are similar in appearance, VLU sores either heal slowly or don’t heal at all, while stasis dermatitis occurs when blood can’t flow properly and pools in the legs. Though it is not the case for everybody, venous ulcers can often occur in people who have stasis dermatitis.
Find out more about the science of veins, the benefits of living a healthy lifestyle, and preventive care for your vascular health and more by reading Dr. Naar’s health blog!
Who is Most at Risk?
There is a significant list of risk factors that can increase your chances of developing VLUs, which all patients should be aware of.
- Age 55 or older
- Family history of CVI
- Higher body mass index
- History of pulmonary embolism
- History of superficial or deep vein thrombosis
- Skeletal or joint disease in lower extremities
- Multiple pregnancies
- Parental history of ankle ulcers
- Physical inactivity/sedentary lifestyle
- Severe lipodermatosclerosis (subcutaneous fat inflammation)
- Venous reflux in deep veins of the lower extremities (3)
Preventing Venous Ulcers
Your health should be one of your main priorities in life. One of the key goals of maintaining a healthy lifestyle is so that we can prevent diseases and conditions which may have a negative effect on our quality of life. Dr. Naar prioritizes preventive steps to combat the occurrence of venous ulcers and recommends the following.
Quit Smoking
In no uncertain terms, if you smoke, stop. Nicotine causes blood vessels to narrow and constrict, limiting the amount of blood available to your vital organs and extremities, increasing your chance of developing cardiovascular disease. (4)
Lose Weight, Maintain Weight
There are many undesirable side-effects of being overweight or obese, one of which is poorer vascular health. Limit your chances of developing varicose veins, venous ulcers and other uncomfortable conditions, by losing weight and maintaining a healthy weight in a controlled, gradual way with advice and personalized guidance from a licensed physician or dietician.
Exercise Regularly
This point may go without saying, but it is vital to your cardiovascular health to stay active, completing at least 30 minutes of activity daily, whether that’s taking a long walk, swimming, hiking, or gym-based exercise.
Keep Moving
Sedentary work and home lifestyles can leave us feeling as though we don’t move around enough. Indeed, not being active is another reason why patients develop vascular conditions, particularly varicose veins.
Elevate Your Legs
If you suffer from CVI, or if you are predisposed to venous ulcers because of hereditary, medical, or lifestyle factors, you can reduce the possibility of developing venous ulcers by elevating your legs for a short time after you have been standing for long periods.
Don’t Put Off Vein Treatment
Left untreated, varicose veins can cause pain and discomfort. The impact poor circulation and varicose veins can have on your daily life can be significant if you leave them too long. If you have conditions such as these, they can put you at an increased risk for serious health conditions, deep vein thrombosis (DVT), and venous ulcers, which can impact your quality of life. In turn, failure to treat venous ulcers early poses inherent risks and is associated with the following complications.
- Cellulitis (a potentially serious bacterial skin infection)
- Osteomyelitis (inflammation of bone or bone marrow)
- Malignant Change (the series of steps prior to cancer development)(2)
If you are prone to spider veins, varicose veins, and VLUs, speak to expert vascular surgeon Dr. Naar at a consultation. Residents of Westlake and the surrounding area can contact Premier Vein Clinic at (440) 641-0433 to book an appointment.
Treatment Options for Venous Ulcers & Stasis Dermatitis
At your personal consultation, Dr. Naar will visually examine the site of your venous ulcers and select one or a combination of the treatment options below.
Conservative Management:
Multilayer compression bandaging has been identified as the gold standard in the treatment of venous leg ulcers, (5) and can be combined with other compression therapy in what is known as conservative management.
- Compression Therapy – Compression therapy uses hosiery, bandages, and compression technology systems to manage venous ulcers. A patient-specific mix of cushions, pads, bandages, drugs (such as zinc oxide), foam, and gel dressings are also used in order to ensure the best possible outcomes for patients. (6)
- Dressings – Hydrocolloid, hydrogel, and low adherence absorbent dressings can be used to protect venous ulcers during the healing process.
Medications:
- Pentoxifylline – Pentoxifylline is part of a family of drugs called hemorheological agents. It helps blood flow through narrow blood vessels more easily by reducing its viscosity (thickness) and can be used to mitigate the effects of venous ulcers. A research review found pentoxifylline to be effective in treating venous ulcers with or without compression therapy compared to placebo or no treatment. (7)
- Antibiotics – Vascular clinicians may employ antibiotics to aid the healing of leg ulcers that are judged to be clinical infections. Doctors must use antibiotics sparingly to prevent antibiotic-resistant microbes from developing, lessening the drugs’ effectiveness.
- Other Medications – Antimicrobials, antiseptics, chlorhexidine, iodine, and other medications may be incorporated into a leg ulcer treatment plan.
Debridement:
- Tissue Removal – One key aspect of treatment for patients with more serious leg ulcers is debridement. Debridement of the wound involves one of a handful of methods to remove necrotic tissue from the wound.
Surgical Management:
- Sclerotherapy – In a sclerotherapy procedure, a skilled vascular surgeon can treat varicose veins and spider veins, but it can also be used when combined with other therapies to fight venous ulcers. Percutaneous (through the skin ) foam sclerotherapy is an effective technique to manage venous ulcers when performed in conjunction with endovenous ablation.(8)
- Endovenous Ablation – When combined with techniques such as sclerotherapy, endovenous ablation is a safe, effective, and less traumatic method of ablating deficient perforated veins. (9)
Personal Consultation with Dr. Naar

During your personal consultation, Dr. Naar will ask you to provide details about your past medical history and experience with venous ulcers. After this, he will perform a non-invasive evaluation of the area for treatment. At this time, he will formulate a personalized treatment plan to help your venous ulcers heal in a timely, effective manner. Call Premier Vein Clinic at (440) 641-0433 to address your vein issues today!
Cost
Dr. Naar provides the highest quality vascular care to all of his patients. The complexity and length of your individualized treatment plan will determine how much your VLU treatment will cost. At Premier Vein Clinic, transparency regarding treatment outcomes and patient goals are priorities. Patients should be informed that the recurrence rate for VLUs is high, so multiple ongoing treatments and a variety of approaches may be necessary to achieve the desired goals.
FAQ
If I have varicose veins, could I get venous ulcers?
If you have varicose veins, this may increase the likelihood of you developing venous ulcers. Additional health factors also play a role, with incidences of venous ulcers higher in patients with conditions such as: a family history of chronic venous insufficiency (CVI), being over 55, having a higher body mass index (BMI), having a history of pulmonary embolism, and a higher number of pregnancies in women. (3)
What are venous ulcers?
Venous ulcers are sores that won’t heal and swelling around your ankles caused by insufficient blood flow and venous insufficiency. They are usually found between the knee and the ankle, though most cases occur on or around the ankle.
I have a sore on my ankle that won’t heal. What should I do?
It is important that you see your primary care physician, urgent care facility, or a vascular surgeon as soon as possible. Severe infection as a result of venous ulcers (such as cellulitis) can pose life-threatening risks and should be dealt with quickly to reduce the risk of complications.
How does compression therapy help venous ulcers?
The pressure exerted during compression therapy can improve circulation by forcing blood back into the deep vein system, aiding the healing of active venous ulcers and preventing their recurrence.
Do venous ulcers leave scarring?
As with any wound from trauma or disease, there may be scarring afterwards. There are many factors that determine the severity of scarring, which include your skin type, age, and severity of infection. Speak to a licensed physician for further information on how best to treat leg ulcer scarring.
References
- Vasudevan, B. (2014). Venous leg ulcers: Pathophysiology and Classification. Indian Dermatology Online Journal, 5(3), 366. https://doi.org/10.4103/2229-5178.137819
- Collins, L. G., & Seraj, S. (2010). Diagnosis and Treatment of Venous Ulcers. American Family Physician, 81(8), 989–996. https://www.aafp.org/afp/2010/0415/p989.html
- Susan Bonkemeyer Millan, Run Gan, & Townsend, P. E. (2019). Venous Ulcers: Diagnosis and Treatment. American Family Physician, 100(5), 298–305. https://www.aafp.org/afp/2019/0901/p298.html
- Nicotine Effect on Cardiovascular System and Ion Channels: Journal of Cardiovascular Pharmacology. (2006). LWW, 47(3). https://doi.org/10.1097/01.fjc.0000205984.13395.9e
- Palfreyman, S., Nelson, E. A., & Michaels, J. A. (2007). Dressings for venous leg ulcers: systematic review and meta-analysis. BMJ, 335(7613), 244. https://doi.org/10.1136/bmj.39248.634977.ae
- Berszakiewicz, A., Sieroń, A., Krasiński, Z., Cholewka, A., & Stanek, A. (2020). Compression therapy in venous diseases: current forms of compression materials and techniques. Advances in Dermatology and Allergology, 37(6), 836–841. https://doi.org/10.5114/ada.2019.86991
- Annamaraju, P., & Baradhi, K. M. (2021). Pentoxifylline. PubMed; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK559096/
- Sarkar, D., & Sarkar, D. (2016). Percutaneous foam sclerotherapy for the management of lower extremity venous ulcers. Journal of Vascular and Interventional Radiology, 27(3), S93. https://doi.org/10.1016/j.jvir.2015.12.246
- Donovan, L., (2019, July 29). Endovenous laser ablation continues to benefit healing of chronic venous ulcers. Venous News. https://venousnews.com/endovenous-laser-ablation-ewma/